Head and neck cancer may not be as common as breast or prostate cancer, but it’s one of the most challenging to treat. Its five-year survival rate can be as low as 25%, while its recurrence rate can be as high as 43%.
West Virginia University researcher Raymond Raylman has developed a new technology to improve the treatment of head and neck cancers. The scanner that he and his team prototyped — which combines positron emission tomography and X-ray computed tomography — showed promising results in recent preclinical testing of its performance. In the future, the scanner may lead to equally promising results in clinical testing.
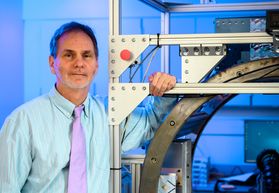
“What makes this system unique is that it has much higher resolution than the standard PET/CT system,” Raylman, vice chair of research for the Department of Radiology and a member of the WVU Cancer Institute, said. “That’s because it’s designed specifically for head and neck cancer imaging. The typical scanner systems are general. They’re designed to image brain tumors, breast tumors, prostate cancer. Instead of doing that, we decided to design one just for head and neck cancer.”
One reason head and neck cancers tend to be so hard to treat is their size. By the time the typical patient receives a diagnosis, “the tumor can often be centimeters in diameter,” Raylman said.
In addition, as physicians plan and execute tumor treatment, they have to avoid sensitive areas nearby, like glands and muscles.
“This system is designed for estimating the edges of the tumor as accurately as possible,” Raylman said. “The more accurately you can assess the size, shape and spread of the tumor, the more accurately — and, hopefully, effectively — you can plan either surgery or radiation therapy.”
He and his team recently tested their system by using it to produce highly detailed images of simulated head and neck cancers. Now they’re seeking regulatory approval to test its performance on 40 cancer patients.
The prototype was made possible by funding from the National Cancer Institute, which awarded the project $1.9 million over five years.
It’s also the result of a collaboration between Raylman and his colleagues in the School of Medicine, advanced manufacturing experts from the Benjamin M. Statler College of Engineering and Mineral Resources’ Lane Innovation Hub, and Xoran Technologies, a manufacturer of X-ray CT scanners.
“Without the Innovation Hub, we couldn’t have developed the PET detectors,” Raylman said. “Their machining is way beyond something we could do.”
“This is exactly the type of collaboration that the Hub was designed for,” Kelsey Crawford, shop manager for the Innovation Hub’s Advanced Manufacturing Lab, said. “Having these capabilities on campus allows researchers from all disciplines to create and iterate their designs, and that’s what we did with this technology.”
Based on data from 2012 to 2016, approximately 44,000 Americans are diagnosed with an HPV-associated cancer every year. About 19,100 of those people are men, and the cancers they’re diagnosed with most frequently are in the head and neck.
One of the biggest risk factors for developing cancer of the head or neck is contracting the human papillomavirus, a very common viral infection that’s transmitted sexually.
According to the Centers for Disease Control and Prevention, nearly everyone will get HPV at some point in their lives. Nine times out of 10, the virus goes away without causing any problems. But in the other 10% of cases, the virus persists and can cause long-term health issues, including cancer.
“HPV-associated cancers in the oropharynx are on the rise, and many of those spread to lymph nodes before they are large enough to be detected,” said The Cancer Institute’s Tanya Fancy, chief of head and neck surgery at WVU Medicine.
“A more sensitive, higher-resolution PET scan like this one can help identify the source of the cancer and allow for a more focused treatment. It would define tumor borders and tumor volume more precisely and show the presence of cancer in lymph nodes in the neck more accurately. Both aspects are crucial to identifying the stage of a patient’s cancer and planning for surgery.”
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number 1R01 CA248492. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NCI or NIH.
MEDIA CONTACT: Cassie Thomas
Director, Communications and Marketing
WVU School of Medicine
304-293-3412; cassie.thomas@hsc.wvu.edu